Intrahepatic portosystemic shunt
8 January, 2020
Case example
A sneaky vessel in the liver
A 14-month-old, female French Bulldog was presented for neurologic signs.
CT findings
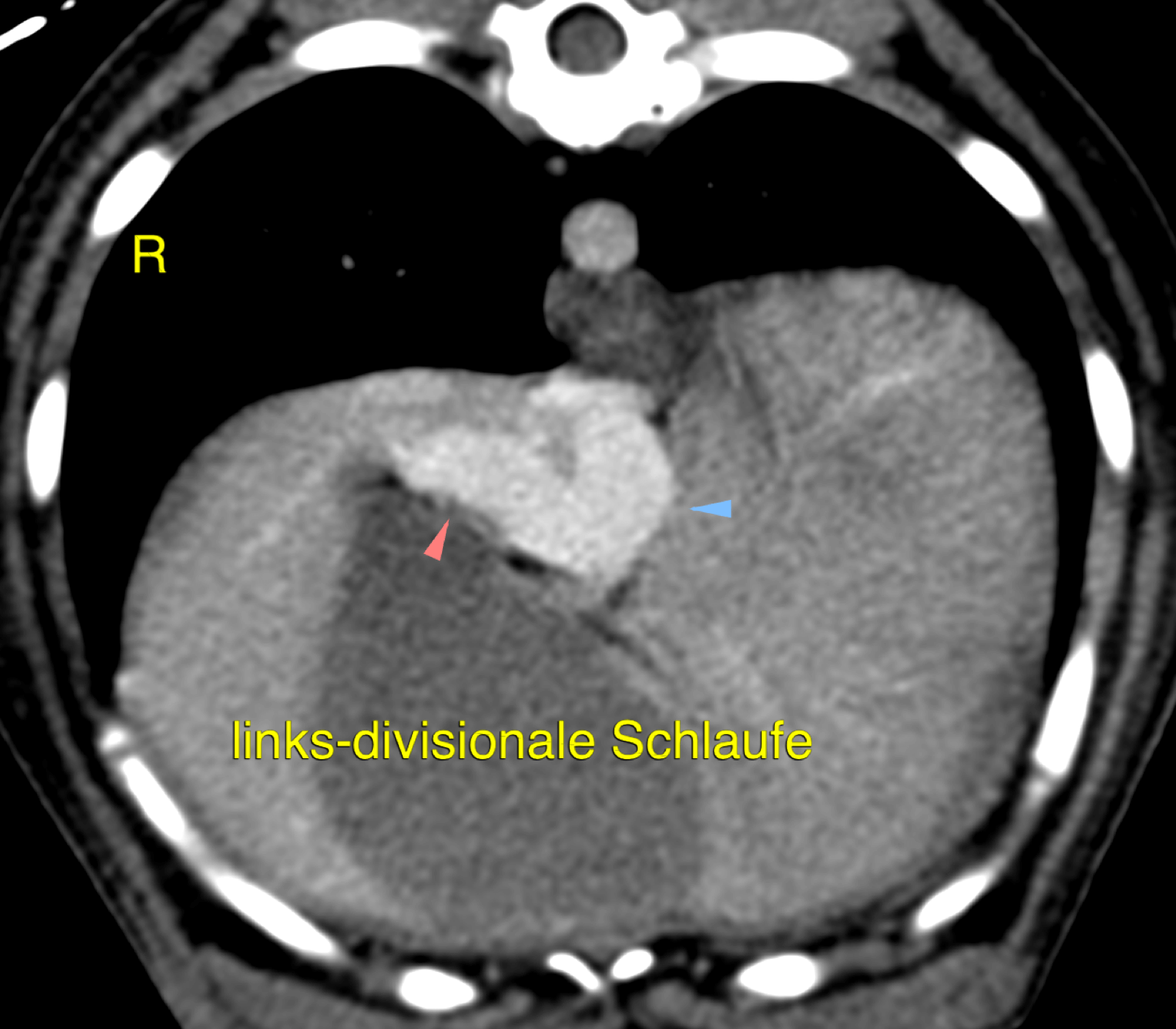
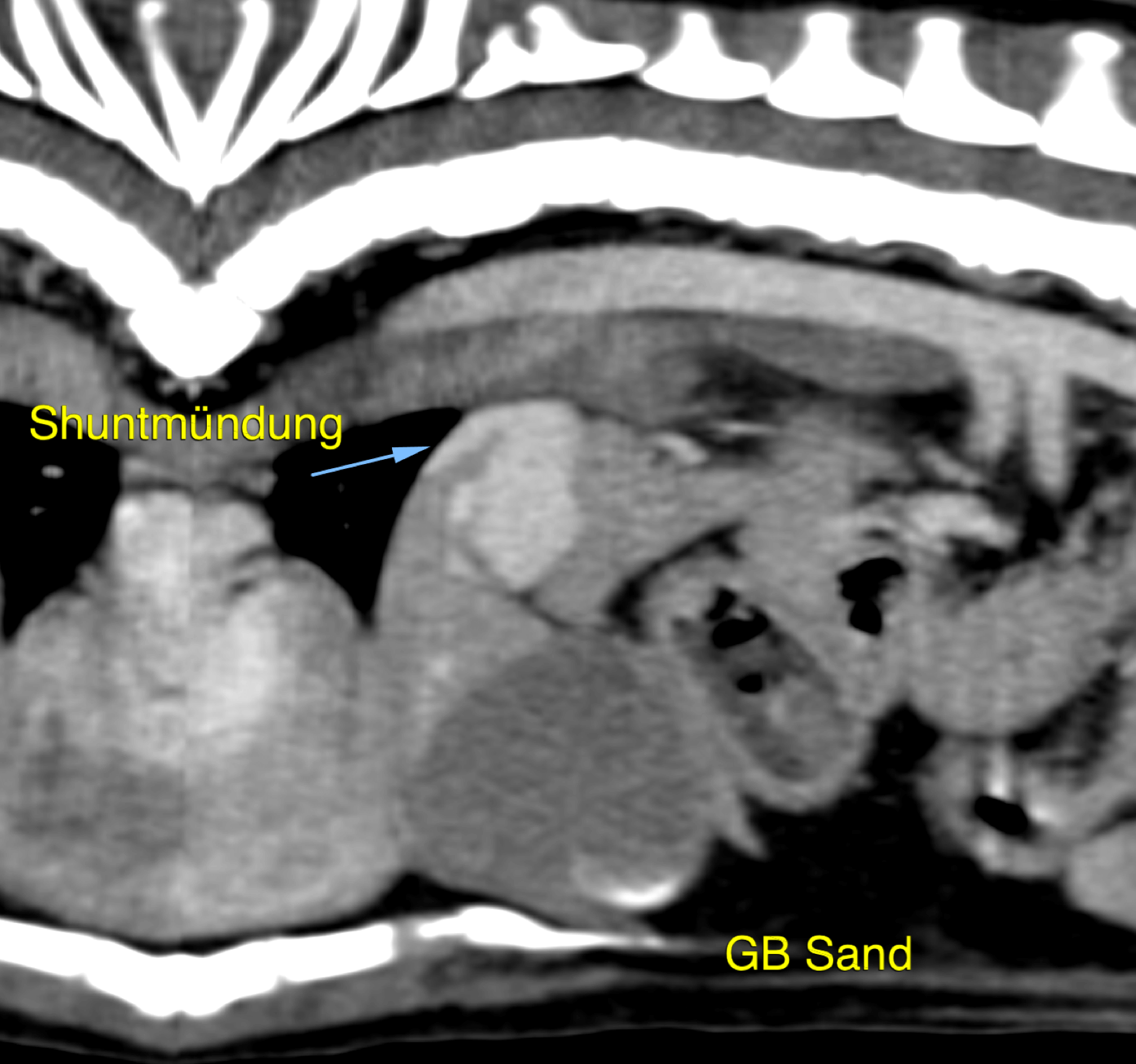
A single cranioventrally coursing anomalous vessel is seen connecting the left intrahepatic portal branch and the caudal vena cava (image 1) entering the patent ductus venosus. (image 2) Additional findings include a decreased liver volume, an increase in size of both kidneys, as well as small mineral attenuations in the region of the renal pelves bilaterally and the urinary bladder lumen.
Conclusions
Single, congenital intrahepatic left-divisional portosystemic shunt (PSS) with secondary microhepatica, bilateral renomegaly, as well as renal and urinary bladder calculi. The reported clinical signs are explained by hepatic encephalopathy.
Learning points
- CT-Angiography (CTA) has been the diagnostic imaging modality of choice for diagnosing portosystemic shunts in dogs and cats. According to Kim et al. CTA is more than five times as likely to correctly diagnose a hepatic shunt in comparison to ultrasonography, even when performed by an experienced sonographer.
- 3 Types of intrahepatic PSS:
- left-divisional: bent tubular shaped vessel draining into the left hepatic vein (patent ductus venosus)
- central-divisional: foramen-like appearance between the intrahepatic portal vein and caudal vena cava; a tortuous vessel has been reported in a cat
- right-divisional: large tortuous vessels draining into the right hepatic vein
- “Comparison of CTA and ultrasonography for the detection and characterization of portosystemic shunts in dogs” Vet Radiol Ultrasound 2013 Vol. 54, No. 6, pp 569-574
- “Anatomy of extrahepatic portosystemic shunts in dogs as determined by CTA in dogs” Vet Radiol Ultrasound 2011 Vol. 52, No. 5, pp 498-506
- “Morphology of congenital intrahepatic portocaval shunts in dogs and cats” Vet Record, Vol 142, Issue 3 1998
Images courtesy of the AniCura Tierklinik Haar, Germany
UPLOAD MEDICAL IMAGES NOW

